Table of Contents
IV. Beware of Caffeine and Alcohol
Osteoporosis Overview
Our bones grow and change as we age. Bones are essential in protecting our organs and providing structure to our bodies. Like every other part of the body, bones are in a constant state of renewal. People reach their peak bone mass in their 30s, and it steadily begins to decline after that. This means that you slowly begin to lose more bone mass than you create. This is a natural part of aging, but for others, this bone loss can be severe and cause life-changing symptoms. Osteoporosis (porous bone) is a disease that occurs when the density and quality of the bones are reduced. [1]
The inside of bones greatly resembles a honeycomb with lots of small holes. In the case of osteoporosis, the holes in the honeycomb grow larger and larger. This compromises the bone and increases the risk of fracturing. Osteoporosis can happen to anyone, but it is more common in postmenopausal women. Around the world, 1 in 5 men and 1 in 3 women over 50 years old are at risk of osteoporotic fractures. The most common areas of a fracture include the hips and spine. Many doctors refer to osteoporosis as the “silent disease” because most people do not know they have it until they experience fractures. Luckily, there are several medications available to lower your risk of developing osteoporosis. If your doctor thinks you are at risk for this bone disease, you may be prescribed Boniva (ibandronate), Fosamax (alendronate), or Evista (raloxifene). Along with these medications, there are several things you can do yourself to help battle osteoporosis. Read on to learn more about foods to avoid when living with osteoporosis. [2] 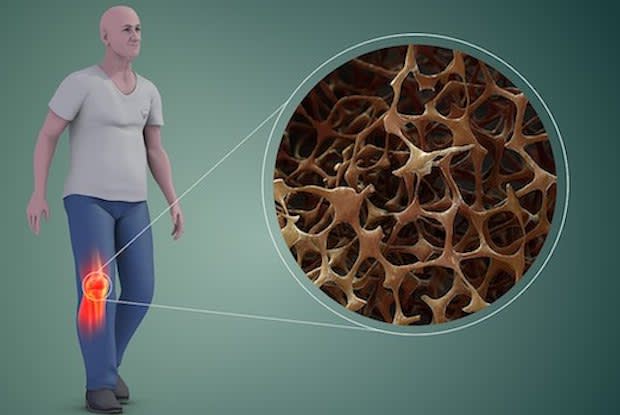
Get savings updates for Fosamax
Avoid Salt
Doctors have found that consuming lots of salt can worsen the condition of your bones. A high-salt diet in postmenopausal women can lead to a loss of bone minerals. On average, Americans consume around 4,000 milligrams of salt a day, when the recommended daily intake is around 2,300 milligrams. [3]
Salt leads to calcium loss, so those with bone loss problems need to lower their salt intake and increase their calcium intake to promote bone growth. Salt is a pesky additive to many foods, so you must keep an eye on ingredient lists. Processed foods like whole-grain bread, fast foods, and breakfast cereals all contain high sodium levels.
Calcium and vitamin D are essential for bone growth. Doctors recommend 1,000 milligrams of calcium a day for adults up to 50 years old. That is the equivalent of three 8 ounce glasses of milk. For females over 50 and males over 70, 1,200 milligrams of calcium is needed, which is about 3.5 glasses of milk. You can get plenty of vitamin D from just getting out in the sunlight and eating foods like saltwater fish, liver, and egg yolks. Eating potassium-rich foods like bananas, tomatoes, and oranges can decrease the loss of calcium in the body. [3]
Watch What You Drink
Soft drinks can also contribute to bone loss. Soft drinks and other carbonated beverages contain phosphoric acid, which leads to increased excretion of calcium in the urine. The occasional soda is okay, but if you are a woman at risk of osteoporosis, you may want to lower your soft drink intake. If you rely heavily on soft drinks as your go-to beverage, you may be more likely to avoid calcium-rich beverages like milk.
Breaking a soda habit can be difficult, but there are several alternatives to soft drinks. You can drink the following beverages to help improve your osteoporosis: It may be surprising to find out that caffeine is another substance that leaches calcium from the bones. Caffeine is not as bad as salt in terms of calcium loss, but it should be monitored regardless. The body loses around 6 milligrams of calcium for every 100 milligrams of caffeine. If a person already lacks calcium in their diet, then a caffeine habit may compound their osteoporosis risk. [3] Doctors recommend limiting your caffeine intake to 300 milligrams a day if you are getting an adequate amount of calcium from other sources, like supplements or milk. One 16 ounce cup of coffee has around 320 milligrams of caffeine. Caffeinated sodas contain around 80 milligrams per can. Interestingly, consuming caffeinated tea does not pose as high a risk for osteoporosis patients as coffee. Doctors think this is because tea contains plant compounds that help protect the bone. If you rely heavily on coffee, you may want to cut back if you are at risk for bone loss. [3] Several studies also show that chronic heavy drinking of alcohol can also have an impact on osteoporosis development. If you consume lots of alcohol while your bones are still developing, it can impact the bone-forming cells (osteoblasts) in the body. Alcohol can hinder bone turnover, bone health, and mineral content. One study on lab rats found that actively growing rats chronically consuming alcohol had shorter femur lengths than those who were not given alcohol. [4] Consuming the right amount of protein can have several beneficial effects on the body. It keeps the stomach full and promotes bone growth. Bones are 50 percent protein, so it is essential for older women at risk for osteoporosis to consume lots of adequate protein in their diet. The suggested daily protein intake for men and women over 19 years old is 0.8 grams per 2.2 pounds. The following foods are natural sources of protein to implement into your diet: Oxalates are natural substances found in many everyday foods. Oxalates can be detrimental to an osteoporosis-friendly diet because they bind to calcium during digestion and are excreted by the body through the stool. Oxalates make calcium unavailable to the body. This reaction results in a loss of calcium, which can worsen osteoporosis. [5] Determining high-oxalate foods can be difficult because many are considered healthy, nutritious, and high in protein. High oxalate foods can include: Soy products like tofu or tempeh can be healthy protein sources, but those with osteoporosis may want to limit their soy intake. [6] Scientists cannot agree on the role of soy in osteoporosis, but some studies show that soy can cause bone strength problems. Soy products can still be consumed as a natural protein source, but it is recommended with a heavy soy diet to consume at least 1,000 mg calcium daily. The content provided in this article is based on thorough research and in some cases, reviewed by a medical professional. Our goal for the information is to provide helpful, general health informational. It is not intended as a substitute for professional medical advice.
Beware of Caffeine and Alcohol
Get That Protein

What are Oxalates?
